Feeling utterly confused? Don’t know what you can do to get over acne?
Don’t worry. You are in the right place. My name is Seppo Puusa, and for the past 5 years I’ve read just about every single scientific paper on acne I managed to get my hands on – well over 1000 by now.
On this page, I’ll explain some of the most important things you have to understand, if you want to get over acne. By the time you are done, you should feel like you finally understand what’s going on in your skin.
It took me over 15 years of living with acne to figure this out. I wrote this page so that others don’t have to wait that long.
Sebum oxidation, the trigger that starts acne
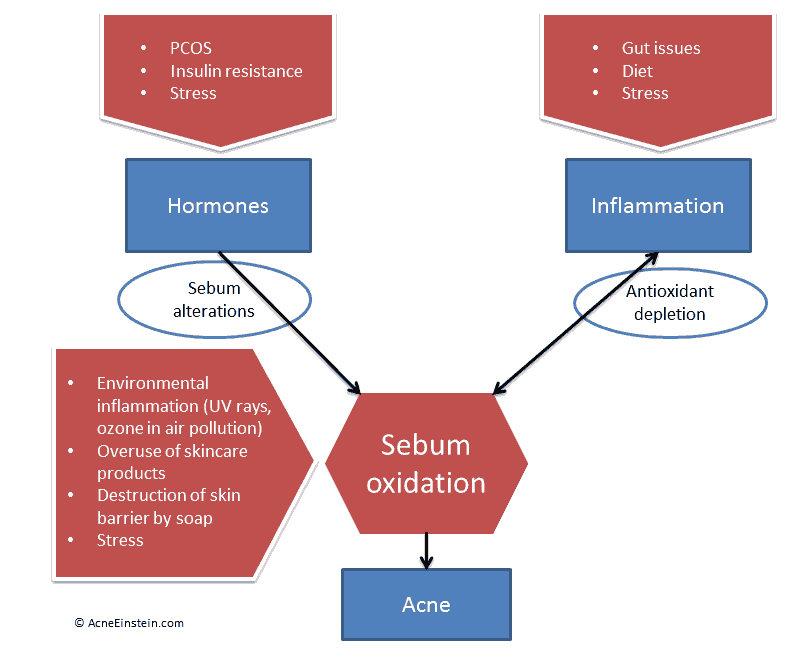
Science on the past decade has conclusively shown that every pimple starts with inflammatory damage to sebum; or sebum oxidation. Everything else you may have heard that causes acne; things like diet, stress, hormones and what not, only create the conditions for sebum oxidation to happen.
This masterpiece of PowerPoint art helps to explain this.
Sebum is a waxy substance composed of triglycerides, fatty acids, and other fatty substance. Out of these, squalene and linoleic acid seem to be the most relevant for acne.
Squalene
Squalene is critical for skin health, and that’s why it’s part of many skin care formulations. However, it comes with a rather nasty downside.
When squalene suffers oxidative damage, it turns into squalene peroxide. Squalene peroxide is massively comedogenic.Animal studies have shown that applying squalene peroxide to rabbit ears causes acne. And the severity of acne is linked to the degree of oxidative damage squalene suffered. In other words, if squalene only suffered minor damage it caused a little bit of acne, but squalene that was badly damaged caused severe cystic acne.
A 2010 review concluded the following:
Comedogenicity of squalene peroxides has been demonstrated in animal experiments in which comedones have been induced by exposing rabbit ears to irradiated squalene. The degree of squalene peroxidation was found to correlate positively with the size of the comedones elicited.
Lipid Mediators in Acne. Monica Ottaviani, Emanuela Camera, Mauro Picardo. Mediators Inflamm. 2010; 2010: 858176. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2943135/
Nobody has studied what happens when you apply squalene peroxide on human skin. However, studies as far back as 50 years found increased levels of squalene peroxides in acne patients. Modern studies have confirmed this (source).
A 2014 study showed that people with mild acne had 79% more squalene peroxide in sebum than people with clear skin. After four weeks of treatment with retinol and vitamin E cream, squalene peroxide levels dropped by 56%. Similarly, the treated areas showed much less hyperkeratinization and inflammation.
Linoleic acid
Linoleic acid (LA) is another important fatty acid. There’s an inverse relationship between sebum production and linoleic acid concentrations; i.e. the more sebum is produced, the lower the LA concentration is. This could explain why people with acne have less LA in sebum. One study showed that people with acne had 65% less LA in sebum than those without acne.
Deficiency in LA causes barrier problems in the follicular duct. Think of the skin pore (follicle) as a tube; LA deficiency causes holes to appear in the wall of the tube and consequently makes them weaker. This makes the follicle more prone to rupture and may result in leakage of substances inside the follicle into the surrounding area. Some of these substances are inflammatory, like bacterial toxins, and likely cause inflammation in the area.
Acne cannot happen without this initial oxidative damage
This oxidative damage to sebum, or lipid peroxidation, is what kicks off a new pimple.
In 2010, Drs. Bowe and Logan wrote a fantastic paper on the role lipid peroxidation plays in acne. They concluded with following:
Indeed, there are indications that lipid peroxidation itself is a match that lights an inflammatory cascade in acne.
Bowe, W. P. & Logan, A. C. Clinical implications of lipid peroxidation in acne vulgaris: old wine in new bottles. Lipids Health Dis 9, 141 (2010). https://www.ncbi.nlm.nih.gov/pubmed/21143923
Everything else you’ve read about acne (blocked pores, bacteria, too much keratin, etc.) follows this initial oxidative damage.
Exposed to squalene peroxide, the cells in the skin drastically increase the production of keratin – a tough protein that binds the skin cells together. Normally dead skin cells are shed off and pushed out of the skin pore one by one. Excess keratin prevents the dead cells from separating properly – so the pore fills up with chunks of dead cells. Too much keratin also makes the pore walls rigid.
Combined with sticky sebum, you have the perfect recipe for blocked pores and the first stage of a pimple. The blocked pore becomes a breeding ground for bacteria. The number of bacteria in the blocked pore grows exponentially, and they start to irritate the skin and cause drastically more inflammation. This is when a pimple starts to get red and painful.
As more sebum and dead skin cells flow into the blocked pore, it eventually bursts – much like a water balloon. The inflammatory material spills out to the surrounding area. This is how big nodules and cysts form.
It’s important to keep in mind that none of this would happen without the initial oxidative damage to sebum.
Understanding how diet and lifestyle affect this
All this talk about microscopic events in the skin does not mean diet and lifestyle wouldn’t affect acne.
Let’s take another look at that masterpiece of PowerPoint art I showed you earlier.
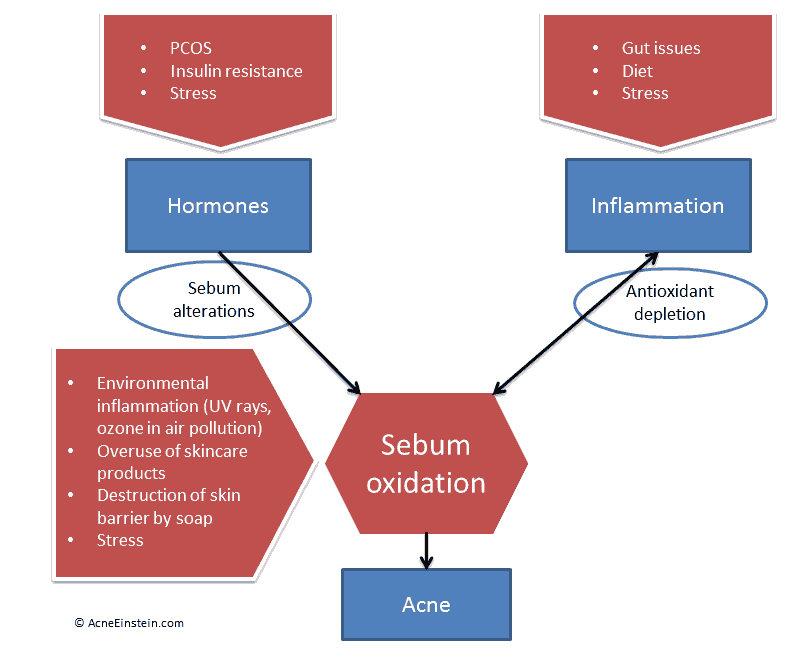
Inflammation and hormonal issues are what sets the stage for sebum oxidation to happen. Briefly, here’s the role each plays.
Hormones
Androgens (male sex hormones, like testosterone) and insulin boost the amount of sebum the skin produces. As the skin produces more sebum, it also produces more squalene.
A 2009 study showed squalene makes up 15% of sebum, while the average for acne patients was 20%. The study also showed acne patients produced 59% more sebum. Putting these two figures together, acne patients had 112% more oxidation-prone squalene than people without acne.
The inverse is true for linoleic acid. The more sebum the skin produces, the less linoleic acid there is in the sebum.
Here’s an easy way to think about this. Imagine a dimmer switch that’s connected to an old lightbulb. The more you open the dimmer switch, the more current goes through the bulb and the more likely it is to burn out.
The same is true for hormones and your skin. As hormone levels increase, so does your risk of getting acne.
Insulin increases sensitivity of the skin to acne causing hormones
Contrary to what most people think, the vast majority of people with acne don’t have abnormally high hormone levels. Some do, but they are a minority.
The difference seems to be in how the skin reacts to the hormones. Studies have shown that acne-prone skin is more sensitive to the androgen hormones that stimulate sebum production. The skin converts various precursor androgen hormones into more potent testosterone and DHT – the hormones that stimulate sebum production the most. All the enzymes required for the conversion are in the skin.
Without going into details, the hormone insulin is one of the keys here. High insulin levels stimulate the release of precursor androgens and increase the activity of the converting enzymes in the skin. Insulin delivers a deadly one-two punch to the skin.
Your diet and lifestyle choices have a huge impact on your hormone levels – and especially on insulin levels. This is why studies have shown that diets that cut sugar and quickly digested carbohydrates can reduce acne.
Inflammation
The skin uses antioxidants to protect sebum from oxidative damage. Antioxidants can neutralize free radicals before they have a chance to damage squalene.
Vitamin E is a major antioxidant in the skin. It’s transported to the skin via sebum. Studies have shown a continuous and much higher flow of vitamin E to the areas of skin that produce more sebum. For example, the sebum collected from the cheeks contained 20 times more vitamin E than the sebum collected from the forearms (source).
Researchers believe that the primary task of vitamin E in the skin is to protect squalene from oxidative damage. There is a very tight correlation between squalene and vitamin E secretion, such that when squalene secretion increases, so does vitamin E secretion.
Shortage of antioxidants is going to leave sebum unprotected and exposed to acne-triggering oxidative damage.
Failure of antioxidant protection in acne patients
Studies comparing antioxidant levels in people prone to acne and those with healthy skin show that the antioxidant protection is overwhelmed in acne patients. For example, one study showed 30% more squalene peroxide and 20% less vitamin E in sebum taken from acne-prone skin (source).
To compensate for the higher demand of antioxidants in the skin, acne patients draw from the body’s antioxidant reserves at a much higher rate than individuals with clear skin. We can see this from studies comparing blood antioxidant and oxidant values between acne patients and people with clear skin. One study showed:
- Vitamin A: 33% lower in acne patients
- Vitamin C: 40% lower
- Vitamin E: 45% lower
- Beta-carotene: 65% lower
This means that the antioxidant system can’t cope with the demand in acne patients. Furthermore, anything that increases inflammation further depletes the antioxidant stores and leaves the sebum even more vulnerable to oxidative damage.
Here’s a list of common things that can cause inflammation and aggravate acne:
- Gut problems
- Stress
- Food allergies and sensitivities
- Allergic reactions
- Smoking
- Stress
Acne types – The first step towards permanently clear skin
So far everything we’ve talked about applies to everyone with acne. However, no two people with acne are the same. What works for one person with acne often doesn’t work for another.
This is where the idea of acne types comes in. Having read a well over 1000 scientific papers on acne and related topics, I’ve come to realize we don’t all suffer from the same acne.
Let me explain.
Yes, hormones and inflammation play a role in everyone with acne. But many different things cause inflammation and hormonal imbalance; such as poor diet, stress, and gut problems.
Regardless of whether it’s caused by stress or gut problems, inflammation still causes acne. But you can’t tell the difference just looking at the skin. In both cases, the person just has ‘acne’.
This is what I mean when I say we don’t all suffer from the same acne. And this is why following what worked for someone else often does nothing for you.
To get over acne, you have to identify the ultimate cause(s) behind your acne – the things that cause hormonal issues and inflammation for you.
You can do that by identifying your acne type.
Not everyone gets acne from drinking milk. Not everyone is stressed because of acne. And not everyone with acne has gut problems. But some do and are.
Acne types help you to identify the cause(s) that are the most likely culprits behind your acne. And guess what? When you look for solutions to those issues, then you are likely to make much more progress with your skin.
Acne types also help to make sense of acne by breaking it down into manageable chunks. For most people, there’s a combination of causes that leads to acne.
The first step towards permanently clear skin
Instead of trying to solve this big and fussy problem called acne, you can solve it in small pieces. For example, it’s common for women to show signs of hormonal and emotional/stress types. So you would go, “OK, I have to make some adjustments to my diet to keep hormones under control, and I should try yoga or meditation to manage stress.”
Much easier and simpler. Because now you have an action plan that’s tailored to your unique situation.
This is why I say that identifying your acne type is the first step towards permanently clear skin.
If this makes sense to you, I urge you to consider Clear for Life, my science-based natural acne treatment course. Clear for Life is built around the idea of acne types. It’s jam-packed with proven diet, lifestyle, and supplement suggestions specific to each acne type. Once you know your acne type, you just mix and match from the suggestions the ones that are relevant for your situation. All the recommendations are based on scientific studies, so you know the advice is proven and reliable. All the dietary advice is ‘real life compatible’ – meaning that you can still go out and have a life while doing this. If that’s something you are interested, you can check out Clear for Life here.
That’s all for now. I hope you found this useful, and that it feels like you are finally getting a handle on what’s going on in your skin.
Best of luck on your journey to clear skin!

Thank you so much for explaining this to me. Everything I have been reading has been total crap. My hormones are so out of whack that it causes frequent seizures and it is horrible! I really do appreciate this information and all the studies you did to put this all together! I will keep following your pages and start sharing these articles. Thank you.
Glad to hear you found this useful, Colleen!
Seppo
I am confused about the squalene issue. I have a Vitamin B3 & 5 gel/cream for acne, that does contain some Vitamin E, hylaluronic acid, and allantoin but it does also contain squalene. Vitamins B3 and B5 are supposed to be good for acne but are you saying it is probably helping break skin out if it contains squalene? Or how would I know if it was oxidizing? I assume the issue is with it oxidizing so how would I know if it is oxidizing? Do you mean in the bottle over time or it automatically does on your skin?
I honestly don’t know whether squalene in skincare products is good or bad for acne. I could see arguments both ways. Squalene oxidizes due to UV radiation or other forms of oxidative damage. This happens in the skin – not in the bottle. I would assume manufacturers add enough vitamin E or other antioxidants into their formulations to prevent squalene oxidation, and that’s why I don’t think it’s automatically bad to have squalene in the product.
This article was so interesting and helpful. This week I started using sweet almond oil on my face once or twice a day, given that it is rich in linoleic fatty acid. I already see a reduction in the redness of my skin, and I am hoping it will eventually fade some of my dark spots from old acne. I do not get too much acne these days, but I have some dark spots that have lingered for years. I plan to check out your Clear For Life page as well. Please let me know if you have any other helpful tips!
hi i am teresa . thank you for explaining the dry skin and acne to me i know now my sugar levels and stress due to deaths of children and also haveing a condition that compro mizes my immune system are to blame . so i know now how to multi task against all the issues i have ,to clear my sore skin . i have recently strated useing alot of all natural things such as vitamin e .coconut oil and coca butter just a few . but i know now to drop the acne treatment and just use ny solid glyerin soap and dove beauty bar and my natural oils and butters . as i am fighting anti ageing and acne . thanks so much i see clear skin in my future.
oh this is teresa again do i need to add rentinol to my skincare ? you can answer me via email. thank you
You mention vitamin E. Isnthis best to be topical or as a supplement? Do you recommend any brands that are better quality than others?
It can work either way. Sorry, but I don’t have any insights into different vitamin E supplements.
I am at the point where milk is the only thing causing me acne. Yet, I love cereal with milk in the morning because it gives me a unique form of protein that helps me focus and have a good day. Is there some kind of milk out there that has the protein but not the sebum?
Soy milk should be ok for guys, but I wouldn’t recommend it for women.
It seems you have gone through a lot of research and different articles on this issue. I will pass it on to others and follow you . It would be more wonderful if you mention how to cope with gut issues and hormonal imbalance which I think is the real culprit in majority of the acne patients. thanks
I’ve been reading your blog posts for the past two days and I have to say I’ve enjoyed reading them very much. I really love the science-based approach since these days, the Internet is filled with every opinion imaginable. I hope I can see results after dramatically reducing sugars and start applying tea tree-based moisturizer. Thank you so much!
Hi Seppo,
I just got off a long-term antibiotic treatment and have been having a lot of digestive/gut issues since, as well as additional acne to coincide with it. I’ve noticed the issues get worse when I consume things like Kombucha, yogurt, etc. Is it possible to have too much “good” bacteria in the gut that may be resulting in digestive issues and acne? If so, what’s the best tactic to getting gut health back to normal? As everything I’ve been reading has been saying to consume things like Kombucha, yogurt, etc and probiotics.
Thanks so much!
Yes, that’s why I don’t recommend probiotics or fermented foods. In some cases, they make gut and skin problems worse. From the feedback I get, it’s much better to go on a low fermentable carb diet for a few weeks to kill of excess bacteria. That usually calms down the gut and the skin.
Regarding the last comment about consuming Kombucha, yogurt, etc. aren’t these considered dairy-based? Could it be that this person may have a sensativety or even allergy to dairy based products rather than to the probiotics? Would a good test be to stop consumption of ALL dairy based foods and supplements & go with a good probiotic capsule instead?
Hey Seppo!!
It’s a huge part of study for the biggest problem called acne!
I do have this issue from long period of time. It actually irritates me. I have the issue of sebum,redness and itchy. I do get at least two per day!even I go with healthy food!.
It’s a sensitive skin with open pores.
Please do suggest me in this great problem on how to avoid it completely both with diet as well with food
Thanks for you time
Hi seppo, I’ve had acne before but I’ve managed it pretty well. I was recently given a course of clindamycin for a possible infection in my mouth. Turns out it wasn’t infected at all so I stopped taking it 6 days in. A week later though I’m experiencing severe acne. Like literally hundreds of pimples on my back alone and it’s been spreading to my chest neck and face the last 2 days. Would you recommend I see a dermatologist about this or from the article do you think probiotics and yogurt would be the best treatment course?
Please don’t recommend Accutane as a save treatment for mild to moderate acne , it should be considered only for severe cystic nodular
Acne , go to acne.org repairing the long term side effects and the horrific long term side effects associated with this chemo drug , it’s heart breaking that they put children and young adults on this poison.
Crohn’s disease is just one of the horrible long term side effects.