Research has uncovered the mastermind molecule behind acne. Mammalian target of rapamycin (mTor) regulates all aspects of acne, including sebum production, cell growth and skin inflammation. It can read the levels of various hormones and nutrients and regulate cell growth and sebum production based on these signals.
In this post I’ll explain the mTor pathway and how it contributes to acne. What’s more important, understanding the mTor pathway and how it’s activated opens up new ways to reduce acne, something we’ll also look at.
What is mTor
Let’s start with a brief explanation of what mTor is. mTor is an abbreviation of mammalian target of rapamycin, a protein that regulates cell growth, cell division and cell survival.
mTor can activate (or turn on) mechanism that promote cell growth, and over-activation of the mTor pathway (medical term for a chain of events where one protein activates the next, ultimately leading to some effect in the body) can lead to excessive cell growth. That’s why mTor has been implicated in some cancers, and why mTor inhibitors are currently being tested as anti-cancer drugs.
Excessively cell growth is also a problem in acne, and that’s why researchers are investigating the role mTor plays in acne and the potential of treating acne by inhibiting the mTor pathway. Let’s look at what scientists have learned so far.
mTOR: The master regulator of acne
Let’s take a moment to review how acne happens.
- Cells called keratinocytes produce too much keratin, a tough protein that binds the cells together. Both inflammatory damage to sebum and exposure to androgens can cause keratinocytes to produce too much keratin.
- Cells called sebocytes produce too much sebum. This process is mainly driven by hormones.
- The combination of too much sebum and keratin creates the ideal conditions for blocked pores to happen. Once a pore is blocked, acne-causing bacteria colonize it, causing an inflammatory pimple.
There’s evidence to suggest that mTOR plays a role in all of these factors.
Keratin production
Animal studies have shown that increasing mTOR activation speeds up keratinocyte growth and accelerates wound healing. Conversely, mTOR inhibitors (tested as anti-cancer drugs) have been linked to slower wound healing.
Sebum production
The paper linking mTOR to acne calls mTOR the ‘central activator of lipogenesis’ (lipogenesis means fat production). Though, as of yet, there are no studies on the effect of mTOR on sebocytes, mTOR has been linked to creation of lipids in other human cells.
mTOR activates the ‘key master transcription factor’ of lipid creation, called SREBP (sterol regulatory element-binding factor). SREBP stimulates creation of fats from precursor molecules in human cells. Because it’s found in nearly all human cells, there’s a good reason to believe it also stimulates lipid production in sebocytes. Inhibition of mTOR deactivates SREBP and thus reduces lipid creation.
This mTOR-sebum connection is probably the reason Accutane suppresses sebum production so effectively. Accutane has been shown to suppress substances ‘upstream’ from mTOR. In other words, it suppresses the substances that activate mTOR and in that way reduces mTOR activity. Green tea catechin EGCG can also suppress mTOR, providing another mechanism for its sebum reducing effect.
Inflammation
There’s evidence that mTOR is linked to skin inflammation. It doesn’t directly cause inflammation, but it’s been shown that the mechanism by which inflammation occurs involves mTOR. And cells where mTOR activity is increased produce more inflammatory cytokines under the same conditions than cells where mTOR activity is not increased. So it looks like mTOR acts as a regulator of inflammation in response to environmental challenges. This is interesting because there’s also evidence that acne prone skin mounts an excessive inflammatory response against P. Acnes bacteria – perhaps it’s possible to reduce this by reducing mTor activation.
So there’s evidence to show that mTOR is a factor in all the processes that lead to acne. Unfortunately this is still a very new area of research and a lot of what I just described is based on preliminary research.
As of yet, there’s no research linking mTOR directly to acne, but there is some research on psoriasis. One study found mTOR (and the substances it activates) activated in psoriatic skin, leading the researchers to suggest that mTOR activation plays a role in psoriasis. Another study showed that Ribosomal protein S6 kinase (S6K1-P), one of the proteins ‘downstream’ from mTOR, was 4-times as active in psoriasis lesions as in normal skin. Downstream in this context means mTOR activates S6K1-P proteins, and the higher activity of these downstream proteins suggests higher mTOR activity.
mTOR and insulin resistance
The effect of insulin, IGF-1 and related hormones on acne is well-known. There’s also evidence that people with acne have some degree of insulin resistance and thus higher than normal insulin level.
Thought we still don’t know all the causes of insulin resistance, excess calorie and sugar intake is one of them. Emerging research suggest that these effects happen via mTOR. Substances downstream from mTOR play a part in the regulatory mechanisms for insulin. They turn off insulin receptors in the cells, so overactive mTOR may lead to insulin resistance. Evidence for this includes:
- One study showed that injection of amino acids into healthy men caused insulin resistance. Amino acids, and especially leucine, are one of the mTOR activators (see below).
- In another study healthy men were given rapamycin, an mTOR inhibitor, and then injected with amino acids. Rapamycin substantially inhibited the insulin resistance caused by the amino acid injection. In this study rapamycin increased the effectiveness of insulin by 17% as compared to placebo.
It seems that mTOR activation not only contributes to acne, but also creates a negative feedback loop by causing insulin resistance that leads to even higher mTOR activation.
mTOR: The point of convergence in acne
mTOR seems to be the point where separate acne causes come together.
This image, I hope, explains the two pathways to mTOR and its role in acne. As a disclaimer I want to say that my understanding and explanation of this may have some holes. The paper I gathered this was very technical and I struggled to understand it. So do forgive me if I don’t get all the technical details correct, but I know that the overall conclusion and the big picture are correct.
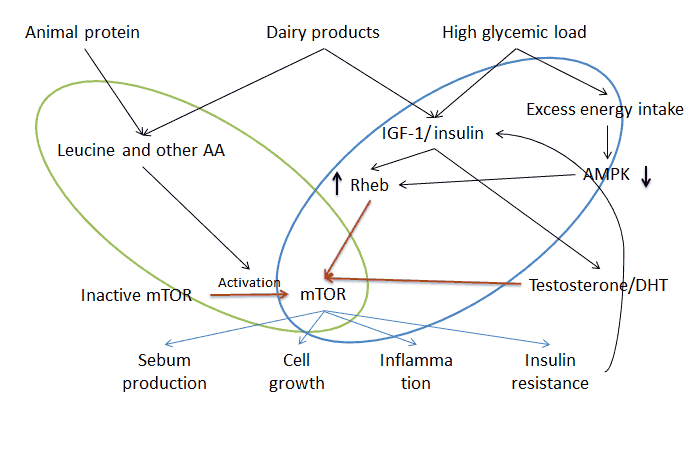
There are two parallel pathways that lead to mTOR activation, marked with the blue and green circles in the image.
- Inside the blue oval we have the insulin/IGF-1 pathway. Insulin and IGF-1 increase Rheb protein activity in the cell. Rheb in turn interacts with and activates mTOR proteins. There’s also another route in this pathway. In response to excess energy intake the enzyme 5′ adenosine monophosphate-activated protein kinase (just AMPK among friends) levels drop. This reduces Rheb inhibitors, with the net effect of increasing Rheb activity and thus leading to higher mTOR activation.
- Inside the green oval we have the amino acid (AA) dependent pathway. For mTOR to be active it needs to interact with Rheb proteins, but Rhebs are only located in certain parts of the cell. Amino acids, and especially leucine, move mTOR from other parts of the cell into areas where Rheb proteins are. So they activate inactive mTOR.
Somewhat related to the insulin/IGF-1 pathway is the effect of androgens (mainly testosterone and DHT) on mTOR activity. The researchers haven’t figured all the ways androgens and mTOR work together, but here’s what is known. Testosterone has been shown to increase the activation of mTOR, and the growth enhancing effect of testosterone is mediated by mTOR (at least in some cell lines).
DHT on the other hand can increase the cellular update of amino acids. This is good news for bodybuilders, but bad news for people with acne and oily skin. It’s been shown that amino acid leucine is an important precursor in lipid production. In plain English, your skin cells turn leucine into sebum.
Both pathways are required for maximal mTOR activation
According to the paper Dietary intervention in acne – Attenuation of increased mTORC1 signaling promoted by Western diet, both of the above mentioned pathways are required for maximal mTOR activation.
From the paper:
“These two synergistic major pathways of mTORC1 activation explain why either insulin/IGF-1 signaling or amino acid signaling alone is not sufficient to reach maximal mTORC1 activation. Insulin is not able to activate the mTORC1 pathway when cells are deprived of amino acids.”
It’s been shown that when cells are depleted of glucose or leucine mTOR activity drops rapidly. This could give us more ways to control acne.
What does this mean?
So far this post has been very theoretical. Probably because I’m a geek who likes to understand how things work. But let’s switch gears and see what this means and how we could use this knowledge to beat acne.
The above mentioned paper makes 4 dietary recommendations:
- Reduction of overall caloric intake
- Reduction of high glycemic index carbohydrates
- Reduction of dairy products
- Reduction of leucine-rich proteins
Most of those recommendations are old news already, but this theory further explains why dairy products are so bad for the skin, they hit both of the mTOR pathways. Dairy products spike insulin and IGF-1 levels more than most foods, with the exception of high glycemic index carbohydrates, and dairy products are high in leucine.
This theory also explains why the combination of whey protein and branched amino acid supplements is so bad for acne-prone bodybuilders. Whey stimulates insulin levels and is very high in leucine, and branched chain amino acids provide abundant leucine for the other pathway.
Further suggestions
Here are some new points I concluded from this research:
- Fat seems to be the safest macronutrient for your skin. Protein and carbohydrates both increase insulin level and most protein sources are also high in leucine. Fat has no effect on insulin level and doesn’t contain leucine or other amino acids. So it makes sense to emphasize fat in your diet, especially monounsaturated fats (like olive oil). There’s some evidence to suggest that saturated fat may cause insulin resistance and inflammation when eaten in large amounts, but I wouldn’t worry about those unless you eat a lot of saturated fat.
- Reducing protein intake could help some people, especially those who haven’t seen benefits from switching to paleo-style diets. In most foods the leucine/total protein ratio is similar, about 8%, so the only way to reduce leucine intake is to reduce protein intake.
- Intermittent fasting could be a way to quickly hack your skin. It’s been shown to quickly reduce both mTOR and insulin levels. It’s not something you would do all the time, but that’s one of the things I would do if I would need to get clear quickly.
- Fruits and vegetables are important for clear skin. Most fruits, and all nonstarchy vegetables, have low to medium GI and very little leucine. They also have natural mTOR inhibitors (subject for a later post) that can inhibit this ‘master regulator of acne’.
- Proper meal timing can help. There’s evidence to show that insulin sensitivity peaks in the morning and decreases during the day. That means eating the carbohydrates in the evening increases your insulin level more than the exact same amount eaten in the morning. See my earlier post for details.
Conclusion
Emerging evidence shows mTor acts as a master regulator protein in acne. mTor can sense hormone and nutrient levels, and increases or decreases its activity based on these signals. It’s the point where insulin and androgen hormones converge in causing acne.
Maximal activation of mTor requires two different signals: high insulin/IGF-1 level and high levels of amino acid leucine. Take away either of these signals and you will reduce mTor activation.
The mTor pathway provides further evidence for the role of high glycemic index carbohydrates and dairy products in causing acne. It also shows it’s possible that foods rich in leucine may aggravate acne. This of course opens new possibilities for treating acne. Perhaps people who haven’t seen good results with low GI diets or carbohydrate restriction can benefit from protein restriction.
Unfortunately much of the research is still preliminary and thus it’s difficult to draw strong conclusions. But I’ll keep an eye on this area. You can also expect further posts on ways to inhibit the mTor pathway.


Seppo,
How does mTor relate to squalene oxidation? Both being involved in the production of sebum and keratin cells? I’m trying to picture it all in my head
MichaelC
Yes and no 🙂 The reason insulin and IGF-1 are so bad for the skin is because they increase the activation of the mTor pathway, which then signals skin cells to produce more sebum and generally make a mess of your skin. It’s the regulator through which hormones and amino acids cause the damage. Does that make sense?
I’ve got a bit of time on my hands so I will read through all the articles in this web site again and I will try reading the original scientific papers. As you have said before, it all comes down to inflammation and hormones so I shouldn’t get too hung up on the finer details of the acne process. I do find it interesting that some people can have very oily skin but never get spots. To me that highlights the individuality of the acne process and the elements within it. It always amazes me how incredibly complicated the human body is and how nature, or the Blind Watchmaker, as Richard Dawkin’s called it, was able to create it
True enough, it comes down to inflammation and understanding mTor and the molecular pathways behind it isn’t that important. The new thing this brings to table is the role amino acids, and especially leucine, play in acne.
I noticed you mentioned intermittent fasting, could you maybe do a blog post about it? I’ve heard a lot of good stuff about it regarding stuff like training and such and I wanted to hear your opinion!
It’s on my list of posts to write. I already did some preliminary research on it and it could be helpful in acne. However, I don’t think I have time to get it done anytime in the near future, probably 2 months down the line could be realistic.
Seppo,
Hallo again.
I was reading this article again after recently finishing a book about the working of cells.
In particularly I was trying to tie this article in with your recent article on Acne Types. I have this thing about trying to create a Grand Unified Theory of Acne in my head. I need to visualise everything.
The MTor protein(which I assume must ultimately link back to errant gene(s) in the nucleus) would appear to play a major role in hormonal acne. In turn linking it to androgens, insulin/IGF-1 and leucine.
However, am I right in saying it’s role is not as pivotal in inflammatory acne with sebum oxidation linking back to gut issues, yeast and food intolerances?
In all cases there is excess sebum and increased skin cell stickiness but in the case of hormonal and inflammatory acne there are different starting points?
I realise an individual could suffer a mixture of the acne types, including emotional acne but I’m trying to establish if the MTor and oxidation routes are separate.
Thanks
MichaelC
You are asking questions that I can’t answer with any degree of certainty. mTor certainly affects hormonal-type acne, but it’s hard to say what effect, if any, it plays on inflammatory and other types of acne. It’s possible it also affects inflammatory signals in the skin, and thus would make people also more prone to inflammatory-type acne. That is, if mTor upregulates inflammatory signals in the skin then it would take less systemic inflammation to trigger acne – I hope that makes sense. But as I said, this is still pure speculation.