Despite only a few studies showing a direct link between stress and acne, there are dozens of studies that show stress adversely affects proximal and distal causes of acne.
Stress and the skin barrier function
The top layer of the skin, called the epidermis, is made of tightly packed, overlapping layers of dry skin cells. These cells are ‘glued’ together with sebum, forming what’s known as the skin barrier. This skin barrier plays a key role as the protector, defender, and gatekeeper of your body. Though finer and thinner than plastic wrap, the epidermis performs remarkably well as a protective barrier for the human body.
The skin barrier serves several vital functions:
- Keeps the water-rich internal organs from drying out by preventing water loss in dry environments
- Acts as a dam to prevent too much water from rushing into the body
- Prevents bacteria and pathogens from entering the body
- Keeps unwanted substances (chemicals, pollution, etc.) out of the body
For these and other reasons, the skin barrier function is a good proxy measure for the overall health of the skin. And indeed, disruptions to the barrier function are a common feature in inflammatory skin conditions, including acne.
The skin barrier’s function is under the influence of the central nervous system, and disturbances there can affect the skin barrier’s functionality. Indeed, several studies show that psychological stress has an adverse effect on skin barrier function. For example, heightened levels of stress are associated with slowed healing of a wound.
A 2001 study looked at the effect of stress on the skin barrier function and recovery in medical students. The researchers damaged the skin barrier by repeatedly attaching a tape to the skin and stripping it out (ouch – for science!). They then measured how long it takes for the barrier function to recover, and further compared the recovery times during periods of high stress (examination) and low stress (return from winter break). Results showed the skin barrier recovered about 30% faster during the low-stress period.
Another study looked at the effect of divorce on skin barrier function and recovery after tape stripping. As in the study on medical students, those with higher levels of stress showed slower skin barrier recovery than their lower-stress cohorts.
Other studies have shown that stress may:
- Increase the permeability of the skin barrier
- Increase moisture loss through the skin
- Slow down the recovery of skin barrier function after an injury (such as an inflammatory pimple)
- Reduce the antimicrobial properties of the skin barrier function and leave the skin more vulnerable to infections
Inflammation
A large body of research shows that stress is a factor in many of our chronic health problems, including heart disease, diabetes, cancer, and depressions. This link is at least partly due to the well-established effect stress has on inflammation. Several studies have established that both acute and chronic stress causes inflammation that can lead to a variety of health problems.
These results show that there is now a convincing body of evidence supporting the notion that acute stress exposure stimulates a slow but steady increase in plasma concentrations of inflammatory markers and that these increases tend to be higher in individuals with less favorable trait or state measures of psychosocial functioning and well-being.
Rohleder, N. Stimulation of systemic low-grade inflammation by psychosocial stress. Psychosom Med 76, 181–9 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24608036
As an example, a 2014 study showed that inflammation levels were about 26% higher in orchestra musicians during a premiere night than during a rehearsal a day earlier.
It seems that the inflammatory response to stress is tied to avoidance emotions, like anxiety and fear. A 2015 study compared the inflammatory response to anxiety and anger. The study showed that anxiety increased inflammation levels whereas anger had no effect.
Social stress can increase inflammation even more than other forms of stress. Social stress involves situations where an individual feels rejected by others. In evolutionary terms, this makes sense, because rejection from one’s tribe often meant death in times gone by.
Unfortunately for acne victims, pimples and social stress often go hand in hand. Feelings of rejection and inferiority are so common among acne patients that they could be a part of the official diagnosis guidelines.
While chronic stress normally suppresses the immune system, in cases where an individual may repeatedly be injured, it can increase immune system activity and systemic inflammation.
Better emotional control reduce inflammatory response to stress
Stress doesn’t affect everyone the same way. Several studies have clearly shown that maintaining emotional control and a positive attitude reduces the adverse effects of stress, including the inflammatory response. A study published in the journal Stress in 2016 concluded.
As such, we conclude that better cognitive control of emotional information specifically predicts reduced inflammatory reactivity to stress in young-adult women. These effects may thus help explain why superior cognitive control is associated with better lifespan health.
Shields, G. S., Kuchenbecker, S. Y., Pressman, S. D., Sumida, K. D. & Slavich, G. M. Better cognitive control of emotional information is associated with reduced pro-inflammatory cytokine reactivity to emotional stress. Stress 19, 63–8 (2016). https://www.ncbi.nlm.nih.gov/pubmed/26581830
Similarly, a study from 2012 showed that maintaining a positive attitude in the face of stress completely eliminated the increase in inflammation.
Self-compassion can also reduce the inflammatory response. In a 2014 study, the researchers divided the participants into high and low self-compassion groups, depending on how self-compassionate they were. The participants were given various stressful tasks and the levels of inflammation were measured before and periodically after the test. This graph shows the results. The grey bar with ‘TSST’ indicates the stressful period.
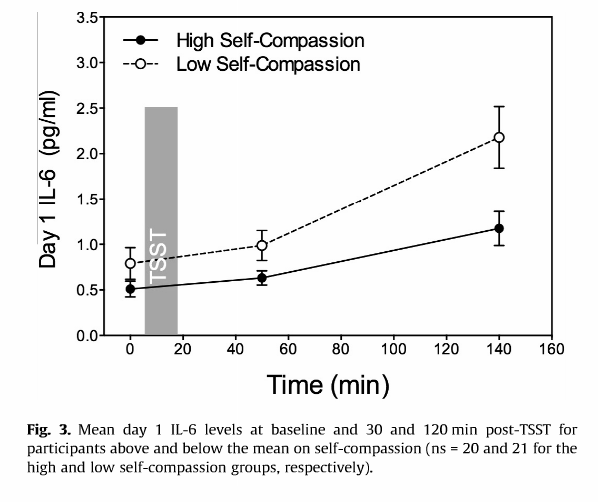
Source: Breines, J. et al. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain Behav Immun 37, 109–114 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24239953
The results clearly show that people who are less self-compassionate have a much stronger inflammatory response to stress, which is one reason I recommend self-compassion exercises.
The results from this study line up with other studies that have shown lower inflammatory response following self-compassion and mindfulness practices.
Stress and the gut
Stress is one of the major factors in gut problems. Without going into details, a 2011 review titled “Stress And The Gut: Pathophysiology, Clinical Consequences, Diagnostic Approach And Treatment Options” concluded that stress:
- Disturbs gut motility (the time it takes for food to pass through the digestive system).
- Changes stomach acid and bile secretion and increasing the risk of bacterial problems in the gut.
- Increases intestinal permeability, i.e. causes leaky gut.
- Slows healing of the intestinal wall after injury.
- Disturbs the bacterial balance in the gut by inhibiting probiotic bacteria and increasing the virulence of harmful bacteria.
- Increases inflammation in the gut.
In other words, stress affects most of the known causes for gut problems.
Stress, emotions and androgen hormones
The adrenal androgens DHEA and DHEAS play a critical role in controlling mood and anxiety. They seem to act as “feel good” hormones and oppose the souring effect of substance P on emotions.
Just as depressed people show higher levels of SP, they also show higher levels of these androgen hormones than non-depressed people. In one study, the researchers measured the DHEA levels of depressed people before and after treatment with antidepressants. They found a significant correlation between depression and DHEA levels: as depression improved, DHEA levels dropped.
In response to the stress hormone corticotropin-releasing hormone (CRH), the adrenal glands secrete both cortisol and DHEA, which the body converts to DHEAS. In one study, the volunteers were subjected to a mock “prisoner of war” situation that included psychological stress as well as sleep and food deprivation. The study found a significant increase in DHEAS levels in response to stress, and that those with higher DHEAS levels showed better mental and physical performance. In another study, in which aviators were exposed to the environmental stress of high-altitude, low-oxygen flight, DHEAS levels doubled in response to the acute stress. Increased androgen hormone levels are not only associated with acute stress, but they are also associated with chronic stress. One study found significantly higher anxiety, depression, and DHEAS levels in people who are bullied at work.
These androgen hormones seem to protect the body against stress-related wear and tear and allow it to perform better under stress. In the mock prisoner of war study, the individuals with higher DHEAS levels performed better both mentally and physically.
In another study, students were subjected to public speaking stress. Exposure to stress increased DHEAS levels by an average of 60%, but what’s really interesting is that those with smaller increases in DHEAS levels reported more negative emotions than people with higher DHEAS response to stress.
So, DHEA and DHEAS seem to help people cope with stress, and the difference in the hormonal response at least partially explains differences in stress tolerance and coping.
Why is this relevant for acne? Because DHEA and DHEAS tend to be the most relevant androgen hormones in female adult acne. The vast majority of studies comparing hormone levels between women with and without acne, show that those with acne have, on average, higher DHEA and/or DHEAS levels – for detailed discussion, please see the hormones page in this section.
The skin contains all the enzymes required for converting these hormones into testosterone and DHT; the two hormones known to stimulate cell growth and sebum production strongly.
In summary, DHEA and DHEAS hormone protect the body against the adverse effects of stress. Unfortunately, these very same hormones can also cause hormonal-type acne.

